Quratis sells TB vaccine worth $1.1B to Indonesia's state-run company - BioWorld Online
Quratis sells TB vaccine worth $1.1B to Indonesia's state-run company - BioWorld Online |
- Quratis sells TB vaccine worth $1.1B to Indonesia's state-run company - BioWorld Online
- Polio: Symptoms, treatments, and vaccines - Medical News Today
- Global health highs and lows in 2019 - Devex
| Quratis sells TB vaccine worth $1.1B to Indonesia's state-run company - BioWorld Online Posted: 17 Dec 2019 12:00 AM PST [unable to retrieve full-text content]Quratis sells TB vaccine worth $1.1B to Indonesia's state-run company BioWorld Online |
| Polio: Symptoms, treatments, and vaccines - Medical News Today Posted: 09 Sep 2016 01:24 PM PDT 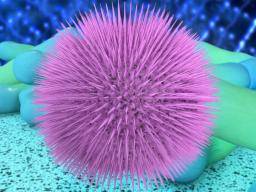 Polio, also known as poliomyelitis and infantile paralysis, is a highly contagious viral infection that can lead to paralysis, breathing problems, or even death. Polio can be classified as occurring with or without symptoms. About 95 percent of all cases are asymptomatic, and between 4 and 8 percent of cases are symptomatic. This MNT Knowledge Center article will look at the causes, symptoms, and history of polio, as well as the steps for eradicating polio completely. Fast facts on polioHere are some key points about polio. More detail and supporting information is in the main article.
Polio is a viral infection that can cause paralysis and death in its most severe forms. It can spread easily from person to person. The World Health Organiation (WHO) aim is to eradicate polio completely and, if this happens, it will be only the third disease to have been beaten in this way, after smallpox and rinderpest. Nigeria, Pakistan, and Afghanistan are the only three countries in which polio has not successfully been stopped. The reach and spread, however, has been reduced in these areas over time. The WHO hopes to achieve the complete eradication of polio by 2018. Polio, in its most severe forms, can cause paralysis and death. However, most people with polio do not display any symptoms or become noticeably sick. When symptoms do appear, they differ depending on the type of polio. Symptomatic polio can be broken down further into a mild form, called non-paralytic or abortive polio, and a severe form called paralytic polio that occurs in around 1 percent of cases. Many people with non-paralytic polio make a full recovery. Unfortunately, those with paralytic polio generally develop permanent paralysis. Non-paralytic polio symptomsNon-paralytic polio, also called abortive poliomyelitis, leads to flu-like symptoms that last for a few days or weeks. These include: Paralytic polio symptomsParalytic polio affects only a small percentage of those invaded by the polio virus. In these cases, the virus enters motor neurons where it replicates and destroys the cells. These cells are in the spinal cord, brain stem, or motor cortex, which is an area of the brain important in controlling movements. Symptoms of paralytic polio often start in a similar way to non-paralytic polio, but later progress to more serious symptoms such as:
Paralytic polio may also be classified as:
Complications and post-polio syndromePost-polio syndrome describes a cluster of symptoms that affect up to 64 percent of all polio patients. It occurs several years after polio has passed. On average, post-polio syndrome occurs 35 years after the infection. Signs and symptoms include:
Post-polio syndrome is a slow, progressive disease. There is no cure, but it is not infectious or contagious. Polio diagnosisPolio is often recognized because of symptoms, such as neck and back stiffness, abnormal reflexes, and trouble with swallowing and breathing. A doctor who suspects polio will perform laboratory tests that check for poliovirus by examining throat secretions, stool samples, or cerebrospinal fluid. There are two vaccines available to fight polio:
IPV consists of a series of injections that start 2 months after birth and continue until the child is 4 to 6 years old. This version of the vaccine is provided to most children in the U.S. The vaccine is made from inactive poliovirus. It is very safe and effective and cannot cause polio. OPV is created from a weakened form of poliovirus. This version is the vaccine of choice in many countries because it is low cost, easy to administer, and gives an excellent level of immunity. However, in very rare cases, OPV has been known to revert to a dangerous form of poliovirus, which is able to cause paralysis. Polio vaccinations, or boosters, are highly recommended for anyone who is not vaccinated or is unsure whether they are. Because there is no cure for polio once a person develops the virus, treatments are focused on increasing comfort, managing symptoms, and preventing complications. This can include bed rest, antibiotics for additional infections, painkillers, ventilators to help breathing, physiotherapy, moderate exercise, and a proper diet. Historically, a person who developed lung paralysis due to polio was placed into an iron lung, a device that would push and pull chest muscles to make them work. However, more modern portable ventilators and jacket-type ventilators are now used instead. Humans have observed the effects of polio for hundreds of years, if not thousands. The relatively recent history of outbreaks in both the United States and Europe has led to an allocation of resources with which to fight the disease. Throughout history, polio epidemics have led to the deaths of many thousands of people around the world. In 1916, for example, over 6,000 people died of polio in the U.S. However, it wasn't until 1953 that Jonas Salk developed the first polio vaccine, which has led to the widespread prevention of poliomyelitis. Although polio has essentially been eradicated in the U.S. since 1979, and in the Western Hemisphere since 1991, children and adults in Afghanistan and Pakistan are still battling the disease. The polio virus usually enters the environment in the feces of someone who is infected. In areas with poor sanitation, the virus easily spreads from feces into the water supply, or, by touch, into food. In addition, because polio is so contagious, direct contact with a person infected with the virus can cause polio. Individuals who carry the poliovirus can spread it via their feces for weeks, even if they have shown no symptoms themselves. Once the virus has entered an individual, it infects the cells of the throat and intestine. The virus stays within the intestines, before spreading to other areas of the body. Eventually, the virus moves into the bloodstream where it can spread to the entire body. As is the case with many other infectious diseases, people who get polio tend to be some of the most vulnerable members of the population. This includes the very young, pregnant women, and those with immune systems that are substantially weakened by other medical conditions. Anyone who has not been immunized against polio is especially susceptible to contracting the infection. Additional risk factors for polio include:
Vaccines are the main way to prevent polio. However, other methods of limiting the spread of this potentially fatal disease include:
Be sure to receive a vaccination before traveling to an area that is prone to polio breakouts. You can check for up-to-date information about these areas on the Centers for Disease Prevention and Control (CDC) website. |
| Global health highs and lows in 2019 - Devex Posted: 23 Dec 2019 12:00 AM PST  MANILA — Global health organizations faced immense challenges in 2019. Ebola remains a concern in the Democratic Republic of the Congo, and health authorities across the globe struggled to contain multiple disease outbreaks, including those that could have been easily prevented with vaccines. Amid the challenges, there were also quite a few bright spots, from disease eradication to successful replenishments. Here are some of the biggest global health events of 2019. Which one grabbed your attention? 1. Ebola, a global public health emergencyCatch up on our coverage of the Ebola outbreak. After months of deliberations, on July 17, the World Health Organization finally declared the Ebola outbreak in DRC a public health emergency of international concern. By November, a significant reduction in cases raised hopes that the outbreak was near containment, but that was crushed with the resurgence of violence in Beni in late November. The violence caused disruption in the response, some staff relocations, and the deaths of three Ebola responders. Following the violence, WHO again saw an uptick in cases, with 27 new confirmed cases from Dec. 4 to 10, compared to an average of seven cases in previous weeks. 2. Large-scale HIV infection of children in PakistanIn April, a town in Sindh Province, Pakistan, captured the world's attention with a jump in reports of HIV cases among children in Larkana district. Mass screenings later confirmed widespread infection that experts traced to questionable health practices in the area, such as rampant reuse of syringes, unscreened blood transfusions, and high numbers of unqualified medical personnel. A study published in The Lancet on Dec. 19 revealed a total of 930 people tested positive for HIV in the screenings between April and July — 79% of whom were children aged 5 years or younger. 3. Disease outbreaksWhile Ebola in DRC remains the biggest health emergency, there were also a number of disease outbreaks health authorities and aid agencies raced to contain during the year, including dengue, yellow fever, polio, and measles. There was an increase in polio cases in 2019, including vaccine-derived polio cases types 1 and 2. The Philippines continues to deal with an ongoing vaccine-derived polio outbreak that started in September. Measles outbreaks also continue to be a concern, with 413,308 confirmed cases from 187 WHO member states in 2019. Catch up on our coverage of vaccine hesitancy. The situation reached unprecedented levels in Samoa, where measles-related deaths have reached 76 as of Dec. 18 and the number of cases amounted to more than 5,000 — leading the government to declare a state of emergency. 4. Global Fund replenishmentThe Global Fund to Fight AIDS, Tuberculosis and Malaria secured $14.02 billion in pledges at its replenishment conference in October, after months of campaigning, with advocates making the case for why donors should invest in the multilateral funder. That total included $100 million that French President Emmanuel Macron, Bill Gates, and Bono promised to secure for the fund to meet its replenishment target. The replenishment is seen as a success and evidence of strong donor trust in the fund, which is a major resource of external funding for many countries fighting HIV/AIDS, TB, and malaria. 5. Global Fund's return to North KoreaIn September, the Global Fund board approved a proposed $41.7 million TB and malaria grant for North Korea, and discussions are currently underway with the government regarding implementation. "The Global Fund is ready to launch a new grant for tuberculosis and malaria in DPRK and can proceed when the DPRK government agrees that UNICEF can sign the grant," said a Global Fund spokesman. How is North Korea coping with TB one year after Global Fund grant cuts? In less than a year, about 100,000 TB patients in North Korea dependent on Global Fund-financed drugs will be left with no medicines after the remaining buffer stocks run out by June 2020. For months before the Global Fund decision, advocates questioned and called on the multilateral funder to resume grants in the country where thousands of TB patients rely on its financing for their treatment. The Global Fund closed its grants in North Korea in 2018 because the unique operating environment in the country had prevented it from "achieving the required level of assurance on the deployment of resources and the effectiveness of grants," said Seth Faison, the fund's director of communications. Speaking to Devex in July, advocates called on the fund to immediately resume its grants and place orders for TB medicines as early as September 2019 to avoid drug stock outs in 2020. They said remaining stocks of TB drugs are expected to run out by June 2020, but it takes 9 to 10 months for items to arrive in North Korea, due to U.N. sanctions. 6. UN high-level meeting on UHCUniversal health coverage got its first official moment in the spotlight this year during the U.N. General Assembly in September. The high-level meeting was a chance for governments to commit to guaranteeing health care for all — something that about half the world's population currently lack. Healthy Access: Read more from our series that takes a closer look at the technology, practical solutions, and innovative financing tools driving improved access to quality care around the globe. Governments signed the agreement, which many experts considered ambitious in scope, but hard financing and monitoring of commitments are still lacking. An estimated $176 billion is needed by 2030 for the 54 lowest-income countries to provide affordable health services, according to the World Bank. But financing is only one part of the challenge. There are countries, such as the United States, which have invested in health care systems, but still have yet to see the results of improving indicators on maternal mortality, for example. What's most important now is how individual countries will interpret the UHC agreement and implement their own plans. And in different countries, the results are bound to take on their own forms. Get development's most important headlines in your inbox every day. Thanks for subscribing! 7. Renewed call for malaria eradicationThe Lancet Commission on malaria eradication made a bold statement in its report in September: The world can be malaria-free by 2050 — if certain measures are put in place. Some members of the malaria community have been cautious about putting a timeline on eradication, given past failed eradication attempts that resulted in donor fatigue and disengagement in the effort. Richard Feachem, head of the commission, said they considered these concerns, but believed that setting an aggressive timeline and showing commitment to malaria can actually encourage donors and inspire national governments. 8. Eradication of wild poliovirus type 3On Oct. 24, the Global Commission for the Certification of the Eradication of Poliomyelitis announced another global health milestone: wild poliovirus type 3 has been eradicated worldwide. This follows the eradication of wild poliovirus type 2 in 2015, leaving only the wild poliovirus type 1 in circulation. However, vaccine-derived polio outbreaks continue to pose challenges to polio eradication efforts and detract resources away from Pakistan and Afghanistan, where wild poliovirus type 1 remains endemic. Efforts are underway to develop a novel oral poliovirus type 2 vaccine — that advocates hope to be available in 2020 — to prevent the emergence of circulating vaccine-derived poliovirus type 2 in the future. Polio advocates have warned against complacency in the fight against the disease and have called on donors to be steadfast in their commitment until polio is globally eradicated. Several donors showed their continued commitment during the Global Polio Eradication Initiative's replenishment in November in Abu Dhabi, although the $2.6 billion pledged amount at the event didn't yet meet the GPEI's overall requirement of $3.27 billion to implement its current strategy through 2023. 9. First WHO global report on visionCatch up on our Focus on: Vision coverage of the challenges, solutions, and innovations in eye care and vision. The importance of eye health is often overlooked, but WHO's first world report on vision in October sought to draw attention to the issue. There are at least 2.2 billion people suffering from a form of visual impairment or blindness globally, and that number is expected to increase even more, according to the report. Access to eye care services is an issue, and most of the time patients pay out of pocket for eye care, as it's not often covered in health insurance schemes or coverage is limited. The report underlined the importance for countries to integrate eye care in their national health plans and care packages. 10. WHO restructuringIn March, WHO Director-General Tedros Adhanom Ghebreyesus announced one of the biggest changes in his transformation agenda — a revamp of WHO's senior management structure. The revamp welcomed new officials in key senior posts. Some members of his existing senior leadership team were given new roles, while others were not included. The restructuring saw the creation of new divisions, and in May at the 72nd World Health Assembly, Tedros announced the creation of a WHO Foundation. 11. InvestigationsSome cases that were brought up in 2018 came to a close this year, while others continue. Here are three significant cases: WHO continues to investigate concerns related to its operations in Yemen. Former WHO officials and staff allegedly engaged in corruption and nepotism using aid money meant to alleviate people's suffering in Yemen, according to an AP investigation published in August. Yemen is currently the world's largest and worst humanitarian crisis, according to the U.N., with millions of children suffering from unprecedented levels of hunger and malnutrition. WHO fraud, harassment cases on the rise WHO's Office of Internal Oversight Services is dealing with increased cases of fraud and other misconduct and wrongdoing, raising concerns among member states. UNAIDS whistleblower Martina Brostrom, who in 2018 accused a senior UNAIDS official of sexual assault and whose case eventually paved the way for an independent investigation into UNAIDS culture, was fired this month. The dismissal was due to a separate investigation that concluded that Brostrom, and another staff member, misused UNAIDS resources and committed sexual misconduct. The other UNAIDS staff was also fired. Brostrom plans to appeal her dismissal, calling it an act of retaliation for reporting about the sexual assault, according to the AP. Thomas Frieden, former director of the U.S. Centers for Disease Control and Prevention, and current president and CEO of Resolve to Save Lives, in June settled a case linked to his 2018 arrest after a woman accused him of sexual misconduct. Frieden pleaded not guilty to the woman's accusations, but pleaded guilty to disorderly conduct, a lesser violation, according to STAT News. Amy Lieberman contributed reporting to this article. Printing articles to share with others is a breach of our terms and conditions and copyright policy. Please use the sharing options on the left side of the article. Devex Pro subscribers may share up to 10 articles per month using the Pro share tool ( ). |
| You are subscribed to email updates from "poliomyelitis treatment" - Google News. To stop receiving these emails, you may unsubscribe now. | Email delivery powered by Google |
| Google, 1600 Amphitheatre Parkway, Mountain View, CA 94043, United States | |
Comments
Post a Comment