Dilated Cardiomyopathy
Interstitial Lung Abnormalities In Patients With COPD Linked To Cancer, Heart Failure Risks
Interstitial lung abnormalities (ILAs) in patients with chronic obstructive pulmonary disease (COPD) are linked to lower lung adenocarcinoma rates but higher rates of other cancers and heart failure.
Interstitial lung abnormalities (ILAs) are associated with various comorbidities in patients with chronic obstructive pulmonary disease (COPD), particularly lung cancer, according to a study published in BMC Pulmonary Medicine.1
Although COPD diagnoses typically rely on patient-reported symptoms and pulmonary function tests, chest computed tomography (CT) imaging is often used to further characterize the disease and associated comorbidities.2 COPD frequently coexists with various comorbidities, like cardiovascular disease, lung cancer, and diabetes.3
Chest CT scans can also detect and characterize ILAs, incidental non-dependent abnormalities that affect at least 5% of lung parenchyma in patients without suspected interstitial lung disease (ILD).4 Previous studies linked ILA with a heightened risk for various pulmonary morbidities, like COPD and lung cancer.1
Despite the well-established relationship between ILA and respiratory morbidities, its correlation with non-respiratory comorbidities remains unexplored. Consequently, the researchers aimed to assess the association between the presence of ILA in patients with COPD and their comorbidities, along with their clinical and laboratory characteristics.
Interstitial lung abnormalities (ILAs) in patients with chronic obstructive pulmonary disease (COPD) are linked to lower lung adenocarcinoma rates but higher rates of other cancers and heart failure.Image Credit: Peakstock - stock.Adobe.Com
They examined a retrospective cohort of patients hospitalized with COPD at the First Affiliated Hospital of Xiamen University. Eligible patients were those diagnosed with COPD according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria and were hospitalized between January 2015 and August 2021.
The researchers extracted all data on eligible patients from their medical records. Next, they classified patients based on the presence or absence of ILA. Then, the researchers performed analyses to identify differences in demographic characteristics, clinical profiles, laboratory results, and comorbid conditions between the 2 groups.
The study population consisted of 1131 hospitalized patients with COPD, with males comprising 93.7%. Of these patients, 82.3% were hospitalized due to acute exacerbations, and 60% had respiratory infections; the median hospitalization duration was 8 days. Additionally, 85.6% (n = 962) had emphysema, and 14.6% (n = 165) exhibited ILAs. The 3 most prevalent comorbidities were lung cancer (19.3%), history of tuberculosis (12.7%), and coronary artery disease (9.9%).
After stratifying the study population into groups based on ILA presence, the researchers noted no statistically significant differences in clinical, demographic, or laboratory parameters. However, the one exception was circulating fibrinogen (FIB) and procalcitonin (PCT) levels. Compared with those without ILA, patients with ILA displayed significantly lower levels of FIB (3.82 g/L vs 4.34 g/L; P = .018) and PCT (0.046 ng/mL vs 0.064 ng/mL; P = .005).
Similarly, the researchers found significant differences in the prevalence of several comorbid conditions among patients with and without ILA. In particular, the incidence of lung cancer among those with ILA was about half that of those without ILA (11.5% vs 20.6%; OR, 0.50; 95% CI, 0.30-0.83; P = .006).
Of those with comorbid lung cancer, 198 were diagnosed during hospitalization, and 20 had a prior diagnosis. The researchers found that 8.6% (n = 17) of the patients diagnosed during hospitalization also had an ILA, a rate comparable to that observed in the group diagnosed before hospitalization (10%). Additionally, they further examined the association of ILA with 3 major lung cancer subtypes: adenocarcinoma (ADC), squamous cell carcinoma (SCC), and other lung cancers.
Compared with those without comorbid lung cancer, those with lung ADC exhibited a significantly lower ILA prevalence (OR, 0.32; 95% CI, 0.15-0.71; P = .005). The researchers found a similar trend among patients with COPD and comorbid lung SCC (OR, 0.48; 95% CI, 0.22-1.11; P = .09); however, this was not statistically significant. Conversely, the prevalence of ILA in patients with other lung cancer subtypes was comparable to that in patients without lung cancer.
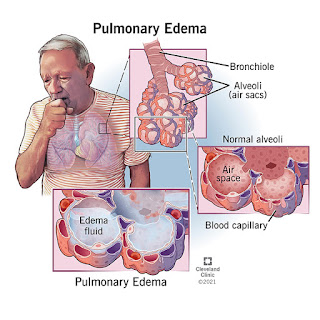
Lastly, the researchers found that the prevalence of cancers other than lung cancers in the ILA group was significantly higher than in the non-ILA group (7.9% vs 3.6%; OR, 2.27; 95% CI, 1.16-4.39; P = .012). Similarly, they discovered heart failure was more prevalent in the ILA group (11.5% vs 6.9%; OR, 1.75; 95% CI, 1.04-3.00; P = .04).
The researchers acknowledged their limitations, including the study population consisting solely of hospitalized patients with COPD, potentially limiting the generalization of their findings. Because of the male predominance among smokers in China, most patients were male, meaning these findings may not be generalizable to female patients. However, they expressed confidence in their findings and suggested areas for further research.
"...Our study demonstrates that the presence of ILA in patients with COPD is associated with multiple comorbidities of the disease, particularly lung ADC," the authors concluded. "Further investigations are warranted to better understand these relationships and their clinical implications."
References
Heart Failure, Pulmonary Hypertension And Cardiology ICU Fellowship Program
In our comprehensive one-year Heart Failure Fellowship program, you will gain robust comprehensive inpatient and outpatient training in the specialty of heart failure.
Our one-year fellowship is offered to PGY-4 level candidates for training focused on heart failure management, pulmonary HTN, with cardiology ICU exposure. Fellows develop the ability to recognize and manage heart failure and understand disease progression. This is a non-standard training (NST) program that is not ACGME accredited.
Our program provides superior cardiology training in a collaborative environment. We have specialty clinics across our medical campus, which is anchored by our 1,200 bed inpatient center UAB Hospital—the eighth largest public hospital in the nation. The hospital is in close proximity to the Birmingham VA Medical Center, UAB Hospital Highlands campus, The Kirklin Clinic, and Children's Hospital of Alabama where fellows also train.
Clinical RotationsOur program offers comprehensive, multidisciplinary training within a collaborative environment. We focus on developing our heart failure fellows by expanding their expertise in areas of advanced heart failure, transplant cardiology, mechanical circulatory support, and pulmonary vascular disease through a combination of inpatient and outpatient care. At the Kirklin Clinic, fellows will engage in specialized clinics for CHF, PH, VAD, transplant, and biopsy suites.
At the Birmingham VA Medical Center, fellows manage a panel of patients longitudinally throughout their training. They also participate in Block model rotations, covering general cardiology, arrhythmia, heart failure, pulmonary hypertension, and elective time including adult congenital heart disease over the three-year program.
Our inpatient services are anchored in our heart transplant ICU, where leading-edge clinical programs for heart transplant, VAD, and PH are managed. Our teams work closely with cardiovascular surgery and interventional/structural cardiologist to address cardiogenic shock using temporary MCS techniques like ECMO, Impella, and TandemHeart. Furthermore, we provide exposure to unique clinical programs such as Cardio-Obstetrics, Cardio-Oncology, and Amyloid/infiltrative cardiomyopathies. Our heart failure fellows aid in supporting our team in managing complex valvular diseases.
Research OpportunitiesOur Heart Failure, Pulmonary Hypertension and Cardiology ICU program works closely with the UAB Comprehensive Cardiovascular Center to foster multi-disciplinary and multi-investigator collaborations and programmatic development in cardiovascular research. We strive to enrich our fellows training experience by exposing them to cutting-edge research in basic, clinical, population, and translational cardiovascular research.
It's not just what you learn. It's also about the people you learn with. Our cardiology fellowship program leaders are dedicated to developing the potential of every talented trainee.Meet our people
Frequently Asked QuestionsAll applications are reviewed by our UAB Cardiology Review Team. All submissions require the following documents:
Current Curriculum Vitae
Professional Photo
Personal Statement
Three (3) total Letters of Recommendation
Certificate/verification from previous residency training
Must be eligible for Alabama Medical License and Alabama Controlled Substance Certificate (all step scores completed at the time of application)
Must be eligible for Federal DEA registration
USMLE or COMLEX Scores
Our program provides benefits and insurance plans available to all fellows at UAB. You can find the list of salaries and benefits for fellows based on PGY level here.
There is no minimum USMLE score requirement. We take the score into account as part of the overall review of an application.
Applications Open and Close — Applications open Decemeber 1 and close December 31.
Applications Reviewed — December
Interview Invitations Released — Mid December
Interviews Begin — December
Fellowship begins — July 1

Send an Email

Joanna Joly, M.D., Associate Program Director
Send an Email
Prevalence Of PH With Left Heart Disease Lower Than Previously Reported
The prevalence of pulmonary hypertension was 12.8% in those hospitalized in 2018 with left heart disease (PH-LHD), a lower percentage than found in previous research. This was among the findings of a study published in Respiratory Medicine.
Previous studies have identified the presence of PH-LHD based on right heart catheterization (RHC), and disease prevalence estimates have ranged from 36% to 85% depending on the type of LHD (62-77% in heart failure with reduced ejection fraction [HFrEF]; 47-62% in HFpEF; 36%-62% in aortic stenosis; and 53%-85% in mitral regurgitation). Investigators conducted a retrospective study of the 2018 Nationwide Inpatient Sample database to determine the prevalence and prognostic influence of different types of PH-LHD. Logistic regression was used to calculate odds ratios for all-cause in-hospital mortality based on PH for each LHD.
The researchers identified 6,270,625 hospitalizations of adult patients in the database aged 18 years and older with a discharge diagnosis of LHD, including heart failure (HF), cardiomyopathies, mitral valve disease, and aortic valve disease. Within the sample, 801,535 patients were diagnosed with secondary PH, with a diagnosis of PH-LHD in 12.8%.
Among patients with HF, the prevalence of secondary PH was 15.0%. Regarding HF subtypes, secondary PH was more prevalent in HFpEF (17.2%) and combined systolic/diastolic HF (18.5%) compared with HFrEF (11.8%). In patients with cardiomyopathies, the prevalence of secondary PH was 14.3%. The percentage was increased for patients with dilated cardiomyopathy (16.8%) vs those with hypertrophic cardiomyopathy (12.6%), or other cardiomyopathy (13.7%).
"
The diagnosis of PH-LHD was associated with worse fatality rates across all forms of LHD, except for HF with reduced ejection fraction.
Regarding valvular heart disease, patients who had mitral valve disease had an increased prevalence of secondary PH compared with those who had aortic valve disease (19.2% vs 13.5%). Secondary PH prevalence was the highest for patients with mitral stenosis (28.5%), and it was reduced in patients with aortic valve stenosis (13.5%).
Patients with secondary PH and HFpEF had especially increased odds of in-hospital mortality (odds ratio [OR], 1.23; 95% CI, 1.17-1.28), compared with those who had HFrEF (OR, 1.04; 95% CI, 0.99-1.10). A stronger effect of secondary PH on in-hospital mortality occurred among patients with hypertrophic cardiomyopathy (OR, 1.42; 95% CI, 1.06-1.89) vs those with dilated cardiomyopathy (OR, 1.13; 95% CI, 0.99-1.29). For valvular heart disease, secondary PH was associated with elevated mortality in patients with mitral regurgitation and aortic stenosis.
Significant predictors of all-cause in-hospital mortality for patients with PH-LHD included age, atrial fibrillation/flutter, cancer, and acute cardiac or extra-cardiac diagnoses. Compared with all other diagnoses, an acute left heart failure diagnosis was associated with an improved outcome for in-hospital mortality in patients with PH-LHD (OR, 0.94; 95% CI, 0.89-0.98).
Limitations include the unknown method of PH diagnosis: it is not known whether the diagnosis was made through RHC or echocardiography. Also, the researchers could not discriminate between PH severity groups, and the analysis was based on hospitalized patients.
"The diagnosis of PH-LHD was associated with worse fatality rates across all forms of LHD, except for HF with reduced ejection fraction," the investigators stated. "This finding should be further explored in future prospective studies."
Disclosure: Some of the study authors declared affiliations with biotech, pharmaceutical, and/or device companies. Please see the original reference for a full list of authors' disclosures.



Comments
Post a Comment