Congenital heart disease in adults - Symptoms and causes
Watch As Gran's Life Is Saved When Doctors Replace Her Artery With 'frozen Elephant Trunk' In Groundbreaking Op
A GRANDMA's life was saved when doctors replaced her artery with a 'frozen elephant trunk' in a groundbreaking op.
Jeanette, 70, was in desperate need of surgery, as her aorta - the body's biggest artery - was diseased and threatening to rupture.
5
Jeanette's artery was replaced with 'frozen elephant trunk'Credit: BBC5
Surgeons at University Hospital Southampton performed the high-risk procedureCredit: BBCThe widow's aortic valve at the top of her heart is also leaking - a defect that can cause heart failure.
"Having an enlarged aorta and a leaky heart is like a time bomb," consultant cardiac surgeon Amit Modi explained.
During an episode of BBC's popular series Surgeons: At the Edge of Life, Amit and his team from the Univeristy of Southampton can be seen performing a high-risk procedure to repair both conditions and give Jeanette a healthy future.
The operation, which can take all day to complete, involves a group of doctors removing and replacing the damaged section of the aorta with a synthetic tube.
The tube, bizarrely called a frozen elephant trunk, is stitched to replace Jeantte's aorta.
Amit can then be seen removing the faulty aortic valve before sewing in a new one made of animal tissue.
"This is not a routine procedure, and the stakes are high," Amid explained.
It amazes me how I can stop and restart the heart every time I do this operation
Amit ModiConsultant cardiac surgeonDuring the procedure, her heart is stopped, and her body is attached to a heart-lung bypass machine, which will oxygenate and pump blood around her body temporarily.
Most read in Health
LEAF IT OUT
M&S 'salad' isn't only 'healthy' meal worse than KFC - as our test revealsSNEEZY DOES IT
TV doctor reveals top 10 common items in home that can cause sneezing fitsEYE SORE
Woman, 22, shares video of eye changing colour after false lashes left her blindJAB OF HOPE
Cancer jab offers hope of a cure as NHS trials vaccines that 'destroy melanoma'The longer Jeanette's heart is not used, the greater the risk it will not start again when she comes off the bypass.
Amit also has to ensure the stitches in the new synthetic aorta are perfect - if they aren't watertight, she could suffer from a fatal bleed.
After six hours in theatre, Jeneattes's heart appears to be pumping, her new valve is working, and the synthetic aorta is carrying blood to her body.
"Even though I've done over 1,500 cardiac procedures, I still feel how miraculous the heart is.
"It amazes me how I can stop and restart the heart every time I do this operation."
5
The op involved removing and replacing the damaged section of the aorta with a synthetic tubeCredit: BBC RecoveryEight months on Jeanette appeared to be recovering well at home surrounded by family.
"Bit by bit, I'm getting back into a normal routine," the gran said.
"I don't worry about the aneurysm bursting."
She added: "I owe Mr Modi a lot; he's given me my life back."
5
Consultant cardiac surgeon Amit Modi led the high-risk procedureCredit: BBC5
Eight months after the surgery, Jeanette appeared to be recovering wellCredit: BBCWhat is heart failure? And what are the symptoms?
Heart failure means that the heart is unable to pump blood around the body properly.
It usually happens because the heart has become too weak or stiff.
It can occur at any age but is most common in older people.
The main symptoms of heart failure are:
Some people also experience other symptoms, such as a persistent cough, a fast heart rate and dizziness.
Symptoms can develop quickly (acute heart failure) or gradually over weeks or months (chronic heart failure).
It most cases, it cannot be cured but the symptoms can often be controlled for many years.
What can cause it?
Heart failure is often the result of a number of problems affecting the heart at the same time.
Conditions that can lead to heart failure include:
Sometimes obesity, anaemia, drinking too much alcohol, an overactive thyroid or high pressure in the lungs (pulmonary hypertension) can also lead to heart failure.
When to see a doctor
See a GP if you experience persistent or gradually worsening symptoms of heart failure.
Call 999 for an ambulance or go to your nearest A&E department as soon as possible if you have sudden or very severe symptoms.
A number of tests can be used to help check how well your heart is working, including blood tests, an ECG and an echocardiogram.
Source: NHS
People Living With Pulmonary Hypertension Call For Better Psychological Support In The Absence Of Awareness Of This Severe Disease
(MENAFN- Andrew Lloyd & Associates) • Over 150 experts and patient representatives from across globe came together at Ferrer's IMPAHCT conference 2024 to address unmet needs of people living with highly debilitating, low-prevalence disease• Patient's voice played even more important role at this year's edition
Barcelona, Spain, April 22, 2024 – Ferrer, an international pharmaceutical company, hosted the 2024 edition of the International Meeting on Pulmonary Hypertension Clinical Treatment (IMPAHCT), that took place in Barcelona, from April 19-20. This event brought together 150 pneumology and cardiology specialists from over 30 countries, reasserting the company's commitment to the research, development and treatment of pulmonary hypertension.1
IMPAHCT 2024 focused on the unmet needs of people living with pulmonary hypertension (PAH) and pulmonary hypertension associated with interstitial lung disease (PH-ILD). Compared to previous editions, this event paid special attention to the importance and role of the patient's voice, which was highlighted at the roundtable entitled: "The patient's perspective in pulmonary hypertension: Opportunities for the future." This gave international experts the opportunity to go beyond uniquely discussing the therapeutic requirements of patients with this disease, to include their needs and desire to achieve a better quality of life.
Hall Skaara, a representative of the European association of patients living with pulmonary hypertension (PHA Europe) and a participant in the roundtable, emphasized the importance of psychological support for individuals diagnosed with PH, in addition to pharmacological treatments: "Several studies2 have indicated that up to 40% of patients develop depression following their diagnosis, due to the heavy burden of living with a chronic and potentially life-threatening disease. This underscores the need to raise awareness of pulmonary hypertension to enable healthcare providers to offer optimal support to their patients."
IMPAHCT 2024 also featured Dr John Wort, Royal Brompton Hospital in London, who shared the results of an epidemiological study designed to determine the prevalence and incidence of PH-ILD across various European countries. During the session, he presented for the first time the findings of the research conducted in the UK.
After analysing the data for the UK, Wort and his associates were able to confirm that pulmonary hypertension associated with interstitial lung disease should be considered a low-prevalence condition, meaning that it affects fewer than five people in ten thousand, and therefore should receive the same attention in the medical community as rare diseases. The study, in which Ferrer participated, is the first on PH-ILD to have used the anonymised health data of millions of people collected at a national level between 2015–2021.
"The robustness of studies presented reveals the urgency of giving greater visibility to pulmonary hypertension; it is a debilitating condition that requires a multidisciplinary approach, like any other rare disease," explains Jorge Cuneo, chief medical officer at Ferrer. "This means we need to raise awareness of its existence to cover the unmet needs of those living with it."
On the second day, the conference held a roundtable in which experts from three different continents, represented by Taiwan, Colombia, Mexico, Germany and Spain, shared their experiences with the disease, with the aim of reaching an overall vision of the best forms of treatment for pulmonary hypertension.
"Ferrer's commitment to organizing the IMPAHCT conference every year reflects our desire to accompany healthcare professionals in improving the quality of life for people living with pulmonary hypertension and their families and caregivers," says Óscar Pérez, chief scientific officer at Ferrer. "In line with our commitment to use business to fight for social justice, this event demonstrates our support for the scientific community through continuing education, and research and development that pursues transformative therapeutic solutions for one of the most serious and debilitating diseases."
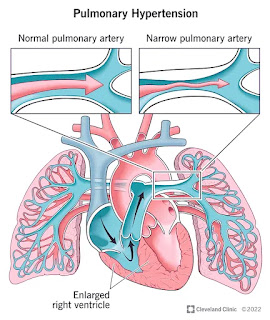
About pulmonary hypertensionPulmonary hypertension (PH) is a condition caused by various diseases and characterized by the development of molecular and anatomical changes in pulmonary blood circulation, which lead to an abnormal increase in pressure in the pulmonary artery (> 20 mmHg).1 It affects approximately 1% of the world's population (a figure that can rise to 10% in people over the age of 65). Nearly 80% of the people living with pulmonary hypertension live in developing countries.3 PH is classified in five different groups, with one of the most common causes being left-sided heart and lung disease.1The development of PH is almost invariably associated with worsening of symptoms such as dyspnoea, fatigue and coughing, among others, and with increased mortality regardless of the underlying pathology.1 While no cures exist for some types of pulmonary hypertension, significant strides have been made in terms of knowledge, therapy and prognosis which have changed the perspective on the disease. As a result, current treatment can help to improve the quality of life of people living with the disease.1
About pulmonary arterial hypertensionPulmonary arterial hypertension (PAH) is just one of over 7,000 rare and ultra-rare diseases diagnosed to date all over the world.4 It is caused by high pressure in the pulmonary arteries, which leads the right side of the heart to work harder than normal and, over time, can trigger right ventricular failure and premature death.1 In Europe, it is estimated to affect anywhere from 15 to 50 people per million, among those of any age, race, condition and sex. It has a higher prevalence in women than men.1
About pulmonary hypertension associated with interstitial lung diseaseInterstitial lung disease (ILD) is a group of pathologies that affect the lungs and are characterized by significant scarring or fibrosis of the bronchioles and alveolar sacs.5,6 The increased fibrotic tissue prevents oxygenation and free exchange of gases between the pulmonary capillaries and the alveolar sacs, and therefore it can be manifested in a wide range of symptoms, including shortness of breath during exercise, difficulty breathing and fatigue.5,6Pulmonary hypertension often complicates the evolution of patients with interstitial pulmonary disease and is associated with worse functional status due to the inability to exercise, greater supplementary oxygen needs, lower quality of life and poorer outcomes.5,6
References1 Humbert M, Kovacs G, Hoeper MM, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension [published correction appears in Eur Heart J. 2023 Apr 17;44(15):1312]. Eur Heart J. 2022;43(38):3618-37312 The impact of pulmonary arterial hypertension (PAH) on the lives of patients and carers: results from an international survey:3 Hoeper MM, Humbert M, Souza R, Idrees M, Kawut SM, Sliwa-Hahnle K, et al. A global view of pulmonary hypertension. Lancet Respir Med. 2016 Apr;4(4):306-22.45 Behr J, Nathan SD. Pulmonary hypertension in interstitial lung disease: screening, diagnosis and treatment. Curr Opin Pulm Med. 2021 Sep 1;27(5):396-404.6 King CS, Shlobin OA. The trouble with group 3 pulmonary hypertension in interstitial lung disease: dilemmas in diagnosis and the conundrum of treatment. Chest. 2020;158(4):1651-1664.
MENAFN23042024006205013440ID1108126125
Legal Disclaimer:MENAFN provides the information "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the provider above.
Recognizing 7 Warning Symptoms Of Congenital Heart Disease In Men: What Happens When You Ignore The Signs?
Late presentation of congenital heart disease (CHD) is very common in low and middle-income countries due to multiple reasons. "Late" means delayed presentation beyond the appropriate age of intervention or surgical repair as per guidelines. Up to 85% of CHD presents late in low and middle-income countries compared to 8-29% in developed countries. Even 10-15% CHD are first diagnosed in adulthood.
In this article, Dr Kuntal Roy Chowdhuri, Department of Cardiology, CMRI Kolkata, tells us more about how ignoring warning symptoms of CHD can have serious health complications, and what needs to be done to stay safe.
Factors Behind Late Presentation of CHDLate presentation of Congenital Heart Disease (CHD) is multifactorial. Financial constraints and lack of awareness are common reasons for late presentations. Other factors such as late diagnosis, ignorance, late referral and fear about cardiac ailments are also contributory.
Consequences of Late Presentation of CHDLate presentation of different CHD has various untoward consequences and it complicates decision-making, surgical repair or intervention and postoperative recovery. It may even cause irreversible damage in the long term and even death. CHD with left to right shunts (i.E Ventricular Septal Defects, Patent Ductus Arteriosus, Aortopulmonary window) which are also known as 'holes' in the heart are very common. If these holes are not diagnosed and repaired at the proper time, it may cause a severe rise in lung pressure (Pulmonary Hypertension).
Pulmonary hypertension poses a unique challenge during operability assessment, surgical planning, postoperative recovery and long-term outcomes. It is heartbreaking to witness patients having simple CHD develop inoperable pulmonary hypertension and experience premature death even today in India.
On the flip side, children with cyanotic heart disease may suffer from inescapable hazards of polycythemia and hypoxia which include headache, stroke, brain abscess, venous thrombosis and cyanotic cardiomyopathy and nephropathy. Timely correction of cyanotic CHD can offer a better quality of life with proper development of organs. Children with single ventricle physiology are the most delicate subset who demand early intervention to protect their single ventricle candidacy. The late presentation is also attributed to severe malnutrition, repeated chest infection and heart failure which appends clinical and financial morbidities.
Diagnosis & Treatment of CHDIt is absolutely important to emphasize early diagnosis and timely treatment of CHD to avoid deleterious complications of late presentation. A multifaceted approach is crucial which includes awareness of the public and physicians at the community level, financial support for treatment and early diagnosis and referral. Early diagnosis can be achieved by Fetal Echocardiography, pulse oximetry screening and availability of echocardiography. Common symptoms of CHD include bluish discolouration of lips and fingertips, 'suck-rest-suck' cycle, repeated chest infection, failure to thrive, shortness of breath on exertion and palpitation. Parents shouldn't ignore these and should get their children evaluated properly. Treatment of CHD may include intervention with device closure, surgical treatment or medical management.
Effects of Timely Treatment of CHDIn the past few decades, tremendous advancement has taken place in the field of congenital and paediatric cardiac care. As a result, early and late outcomes of all simple and complex heart diseases have improved significantly. If treated timely, simple and complex heart diseases can be surgically corrected with about 2-5% and 10-15% mortality risk, respectively. In many simple and complex CHD may lead an almost normal life if treated timely. Activity restriction after CHD surgery is only required in selected high-risk patients and should not be generalised. Social life including pregnancy is possible in most corrected biventricular CHD patients but demands careful pre-conceptional evaluation. Nevertheless, CHD patients should adhere to follow-up visits as advised by their doctors.
ConclusionMisconceptions among the public and physicians regarding CHD symptoms, availability of treatment options and short and long-term outcomes need to be addressed aggressively. Timely treatment is the cornerstone of CHD treatment. Everyone should understand that a baby born with some critical CHD [Obstructed Total anomalous pulmonary venous connection] might need intervention or surgery even at a few hours of life.
Don't Miss Out on the Latest Updates.Subscribe to Our Newsletter Today!
Subscribe Now


Comments
Post a Comment