Pulmonary hypertension: Symptoms, causes, and treatment
Premature Coronary Artery Disease: Symptoms, Treatment, And Outlook
Premature coronary artery disease (CAD) is also called "early onset CAD." It means that a younger adult has CAD, though many of the causes and symptoms of CAD are the same at any age.
In the United States, coronary artery disease (CAD) is the most common form of heart disease. It can affect both younger and older individuals, but, when it affects younger individuals, it's classified as premature CAD.
Premature CAD has many of the same symptoms and risks as CAD in older individuals. When signs or symptoms of CAD appear at any age, it's important to take action.
This article will explain more about premature CAD and what steps you can take to reduce the risk of serious health effects, possibly through medication, surgery, or lifestyle changes.
"Premature CAD" means that a younger adult has CAD. Another term for premature CAD is "early onset CAD."
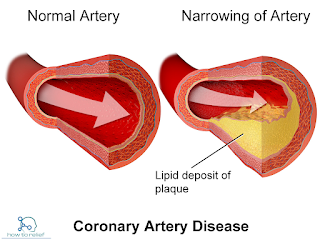
"Coronary artery disease (CAD)" means that there's reduced blood flow in the heart because of a buildup of plaque in the arteries. CAD can be extremely dangerous because plaque buildup can narrow or completely close arteries, causing a heart attack or heart failure.
The symptoms of premature CAD are similar to the symptoms of CAD, and, as mentioned, the first sign many individuals experience is a heart attack.
Symptoms of a heart attack may include:
Even if they don't have a heart attack, many individuals who have premature CAD will experience chest pain or angina. These conditions may occur because the heart isn't getting enough blood, which means that it's also getting reduced levels of oxygen.
Every individual's CAD story is different, but sex may affect the likelihood of experiencing certain symptoms. According to research, females are more likely to experience some of the more atypical symptoms of premature CAD, which may include:
Premature CAD is caused by the buildup of plaque in the coronary arteries. This plaque is made up in part of cholesterol deposits.
Over time, the plaque buildup leads to a narrowing or closing of the arteries, a process called "atherosclerosis." Eventually, CAD can also cause the heart muscle to weaken, which may lead to heart failure.
Risk factors for premature CAD include:
Your ethnicity, sex, and certain genetic conditions may also affect your likelihood of experiencing premature CAD.
There's no cure for premature CAD, but you can do things to reduce their risk of developing CAD. Preventive measures may include:
Medications can also be used to ease the effects of premature CAD on the heart and body. Some medications may be prescribed to lower blood pressure, widen or relax arteries, and decrease the chance of a heart attack, including:
Surgical procedures may be recommended to improve blood flow to and through the heart. These procedures may include coronary bypass surgery or angioplasty and stent placement.
In coronary bypass surgery, a blocked artery is bypassed using another artery or vein in the body.
In an angioplasty and stent placement procedure, an inflated balloon is used to push plaque toward the artery walls and widen the blood vessel. A stent is then placed to help keep the artery open.
Cardiac rehabilitation will likely be necessary if you experience a heart attack or require heart surgery. Rehabilitation may typically include an exercise plan, education on healthy heart practices, and counseling.
Around the world, CAD is the third leading cause of death. It's responsible for 610,000 deaths each year, and 1 in 4 adults younger than 65 years die of CAD, according to 2023 research.
The mortality rate for coronary artery disease (CAD) has decreased over the last 3 decades, but the mortality rate for individuals under 55 years who have CAD has only barely decreased (0.1%) in the last 2 decades.
Additionally, there have been increasing rates of three known risk factors for premature CAD: hypertension, diabetes, and obesity.
More than four-fifths of individuals who have premature CAD also have a risk factor that can be adjusted. These risk factors may include:
Eliminating these risk factors may improve the outlook for people who have premature CAD. This may mean quitting smoking, taking medications to control a health condition, or increasing physical activity.
Premature CAD is a condition in which CAD occurs in males younger than 45 years and females younger than 55 years. It has many of the same symptoms and causes as regular CAD.
If you're showing any symptoms of CAD, such as chest pain, it's important to seek medical assistance regardless of your age. It's also important to make lifestyle decisions that promote heart health at any age.
What Is Diffuse Coronary Artery Disease, And How Is It Treated?
Diffuse coronary artery disease is a subtype of coronary artery disease (CAD) in which larger sections of coronary arteries have a high plaque buildup. It is less common than focal CAD and can be more challenging to treat.
Between 2009 and 2012, CAD affected around 7.6% of men and 5.0% of women in the United States.
This article details the symptoms and risk factors for diffuse CAD, as well as steps a person can take to prevent the condition. It also explores a person's outlook, the complications, diagnosis methods, and treatment options for diffuse CAD.
A 2022 subanalysis suggests that there is no standardized definition of diffuse CAD and that it relies on visual assessment.
However, older research from 2004 defines CAD as one of the following:
The 2022 subanalysis notes that there is also a newer metric to define CAD patterns called the pullback pressure gradient (PPG).
The PPG identifies the focal or diffuse pattern of CAD based on the location and extent of the drops in blood flow pressure along the coronary artery.
This metric provides the pattern of CAD with a numerical value. A value of 0 indicates diffuse CAD, and a value of 1 indicates focal CAD.
Symptoms of diffuse CAD are similar to those of focal CAD. According to a 2023 overview of research, these include:
Some of these symptoms could indicate that diffuse CAD has developed into a life threatening condition, such as heart failure or heart attack.
Anyone with symptoms of a heart attack should seek immediate medical attention. Symptoms include:
Diffuse CAD arises when there is a buildup of plaque in the arteries supplying blood to the heart. A paper from 2015 suggests that diffuse CAD can affect those with:
Other factors that can increase the risk of developing CAD include:
Researchers continue to study other CAD risk factors. Some possible risk factors include nonalcoholic fatty liver disease and rheumatoid arthritis.
Doctors diagnose diffuse CAD using the following tests:
Surgery is an important part of focal CAD treatment. However, the significant buildups of plaque in those with diffuse CAD can make surgery more challenging.
Despite these challenges, a 2019 study notes that the average person with diffuse CAD could benefit from surgery. A 2017 study found similar results.
A surgeon may perform coronary bypass surgery. During this procedure, a surgeon uses healthy blood vessels from another part of the body, such as the leg or chest, and connects them to the blood vessels near the blocked artery. This creates a new route for the blood to flow through.
For those who are unable to undergo surgery, an interventional cardiologist may perform a stent placement. To do this, the healthcare professional will thread a thin tube with an empty balloon attached to the end through a blood vessel.
They will then place the balloon in the blocked artery and inflate it, allowing them to open the stent and place it into position.
Medications can include:
It may not be possible to prevent diffuse CAD with complete certainty. However, taking some steps could reduce the risk of developing this condition.
As the 2023 paper makes clear, some risk factors, such as diet and a lack of exercise, are modifiable. A person may benefit from maintaining a healthy lifestyle, which includes:
CAD is a serious condition and is the most common cause of death in the United States.
According to a 2018 paper, research suggests that people with diffuse CAD have a lower survival rate than people with focal CAD.
However, the survival rate for diffuse CAD varies from person to person. Demographic factors, overall health, and other health conditions can all affect an individual's outlook.
It is important to contact a doctor as soon as possible if a person experiences any symptoms of CAD.
There are many possible complications of diffuse CAD. According to the 2023 review, some common complications of CAD include:
CAD refers to a buildup of plaque in the coronary arteries, which supply blood to the heart. Diffuse CAD is when large sections of the coronary artery have this plaque buildup.
Diffuse CAD can sometimes make treating the condition with surgery or stenting more challenging. It also increases the risk of death from CAD complications, including heart failure and heart attack.
However, a surgeon can treat the condition by performing a coronary bypass. For those unable to have surgery, an interventional cardiologist can insert a stent. A healthcare professional may also prescribe medications such as beta-blockers and ACE inhibitors.
People can take steps to prevent or manage diffuse CAD. These include exercising regularly, not smoking, and eating a heart-healthy diet.
Coronary Artery Disease
Coronary artery disease (CAD; also atherosclerotic heart disease) is the end result of the accumulation of atheromatous plaques within the walls of the coronary arteries that supply the myocardium (the muscle of the heart) with oxygen and nutrients. It is sometimes also called coronary heart disease (CHD). Although CAD is the most common cause of CHD, it is not the only one.
CAD is the leading cause of death worldwide. While the symptoms and signs of coronary artery disease are noted in the advanced state of disease, most individuals with coronary artery disease show no evidence of disease for decades as the disease progresses before the first onset of symptoms, often a "sudden" heart attack, finally arises. After decades of progression, some of these atheromatous plaques may rupture and (along with the activation of the blood clotting system) start limiting blood flow to the heart muscle. The disease is the most common cause of sudden death, and is also the most common reason for death of men and women over 20 years of age. According to present trends in the United States, half of healthy 40-year-old males will develop CAD in the future, and one in three healthy 40-year-old women. According to the Guinness Book of Records, Northern Ireland is the country with the most occurrences of CAD. By contrast, the Maasai of Africa have almost no heart disease.
As the degree of coronary artery disease progresses, there may be near-complete obstruction of the lumen of the coronary artery, severely restricting the flow of oxygen-carrying blood to the myocardium. Individuals with this degree of coronary artery disease typically have suffered from one or more myocardial infarctions (heart attacks), and may have signs and symptoms of chronic coronary ischemia, including symptoms of angina at rest and flash pulmonary edema.
A distinction should be made between myocardial ischemia and myocardial infarction. Ischemia means that the amount of blood supplied to the tissue is inadequate to supply the needs of the tissue. When the myocardium becomes ischemic, it does not function optimally. When large areas of the myocardium becomes ischemic, there can be impairment in the relaxation and contraction of the myocardium. If the blood flow to the tissue is improved, myocardial ischemia can be reversed. Infarction means that the tissue has undergone irreversible death due to lack of sufficient oxygen-rich blood.
An individual may develop a rupture of an atheromatous plaque at any stage of the spectrum of coronary artery disease. The acute rupture of a plaque may lead to an acute myocardial infarction (heart attack).


Comments
Post a Comment