Intravacc's Sabin Inactivated Polio vaccine (sIPV), out-licensed to LG Chem, receives WHO prequalification - PRNewswire
Intravacc's Sabin Inactivated Polio vaccine (sIPV), out-licensed to LG Chem, receives WHO prequalification - PRNewswire |
- Intravacc's Sabin Inactivated Polio vaccine (sIPV), out-licensed to LG Chem, receives WHO prequalification - PRNewswire
- What happens when children go unvaccinated, from those who know - UNICEF Australia
- Vaccines and COVID-19: The latest hopeful research - Medical News Today
- Is it ethical to continue COVID-19 vaccine trials? - Medical News Today
| Posted: 21 Jan 2021 12:00 AM PST
BILTHOVEN, the Netherlands, Jan. 21, 2021 /PRNewswire/ -- Intravacc, a world leader in translational research and development of vaccines, today announces the WHO prequalification for the Sabin-IPV (sIPV) vaccine Eupolio™, developed by Intravacc and out-licensed to South Korean LG Chem in 2014. The vaccine was developed by Intravacc for technology transfer to manufacturers in low- and middle-income countries in the context of the global polio eradication initiative. Eupolio™ received the prequalification status from the World Health Organization (WHO) by the end of December. LG Chem signed a contract with UNICEF to supply $80 million worth of polio vaccine Eupolio™ from 2021 to 2022. The company will supply the vaccine to 70 countries in the Middle East, Africa and Southeast Asia starting in January 2021. Intravacc will receive milestones and low single digit royalties for its considerable role in the development of this vaccine. In a phase III study completed in 2019 with Eupolio™ high neutralizing antibody titres were obtained against both wild-type and Sabin polioviruses, which will also protect against circulating vaccine-derived polioviruses (cVDPV) that make up the majority of polio cases in recent years. WHO prequalification of Eupolio™ is a major milestone in ongoing efforts towards global polio eradication, as it will help close the gap between demand and supply of safe and effective Inactivated Polio Vaccine (IPV) for millions of infants in need of immunization against poliovirus. To reduce the use of the virulent vaccine derived polioviruses, a switch to inactivated polio vaccines (IPV) was desired. Because of the limited supply and relatively high-cost price world-wide of IPV, Intravacc in collaboration with the WHO, initiated the development of a cost-effective manufacturing process for an inactivated poliovirus vaccine using attenuated (Sabin) poliovirus strains (sIPV) to be transferred to local manufacturers. LG Chem is the first manufacturer to bring the sIPV vaccine to the market. Dr. Jan Groen, Intravacc's CEO, said: "This is a great example project in which Intravacc's innovation and knowledge has been the basis of the development of an affordable vaccine that contribute to the reduction of infectious disease burden at a global level. We are confident that this joint effort with several of our license partners will significantly contribute to the polio eradication program." Poliomyelitis About Eupolio About Intravacc's Vero cell platform About Intravacc Contact info Intravacc Mirjam Hartman, Media relations LifeSpring Life Sciences Communication, Amsterdam SOURCE Intravacc, Innovating Vaccines  |
| What happens when children go unvaccinated, from those who know - UNICEF Australia Posted: 13 Jan 2021 12:00 AM PST  Ending polio with Richard, Kinshasa, DR CongoRichard Elaka, 60, is a polio survivor in Kinshasa, the Democratic Republic of Congo's sprawling capital. He was infected at the age of seven and has been moving around on crutches ever since. For more than 20 years, Richard has been a community outreach worker informing parents in the commune of Makala in Kinshasa about the importance of vaccination and the risks of non-vaccination. "I realised that many families don't get their children vaccinated because of a lack of knowledge," he explains. Poliomyelitis, known commonly as polio, is a deadly viral infection spread not only through coughing and sneezing but also though contact with an infected person's faeces. Whilst the majority of those infected with poliovirus will have only very minor flu like symptoms, in its most severe form, polio can affect the spinal cord, causing paralysis and even death. "Vaccination is a gesture of love "In the morning I wake up, I take my awareness materials and go meet families with 0-59 month old children," Richard says. "When I arrive in a family, I make the parents understand that vaccination is a gesture of love that protects the children. When they vaccinate their children, they are protecting them." "For parents who refuse to have their children vaccinated, I explain to them that I am myself a victim of polio. Look at me. If you don't want your children to be vaccinated, you see the consequences. "When a child has polio, he will be disabled for the rest of their life. Your children need to be immunised." |
| Vaccines and COVID-19: The latest hopeful research - Medical News Today Posted: 18 Jan 2021 12:00 AM PST 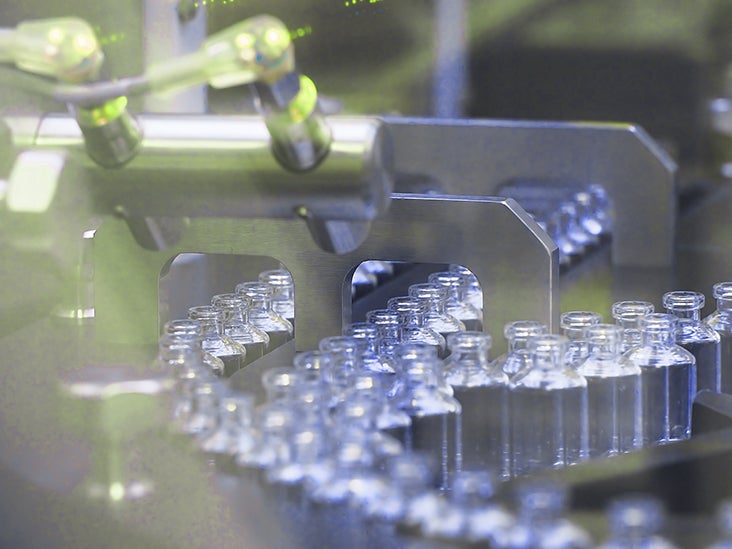 What is the latest in COVID-19 vaccine advances? Can currently authorized vaccines protect against newly emerging SARS-CoV-2 variants? In this Hope Behind the Headlines feature, we examine these and other questions. New, and possibly more contagious, variants of SARS-CoV-2 — which is the virus that causes COVID-19 — are emerging in countries around the world. Add to that the fact that the global number of COVID-19 cases is currently at over 95 million, and it can be difficult to remain optimistic that we will see the end of the pandemic anytime soon. Yet scientists have not stopped working on vaccines, which are key to controlling the spread of the new coronavirus in the long run.
In this Hope Behind the Headlines feature, we look at what experts have to say about whether or not currently authorized vaccines are likely to protect us against new SARS-CoV-2 variants. We also give an overview of a promising vaccine candidate currently under trial, which has recently made the headlines. Experts have explained time and again that in order to contain SARS-CoV-2 and prevent more coronavirus outbreaks in the future, vaccines are of utmost importance. At the moment, there are eight COVID-19 vaccines with authorization in countries around the world. So far, the Pfizer-BioNTech vaccine, which is an mRNA vaccine, has gained authorization for use in 50 countries. These include the United States, the United Kingdom, and the 27 countries that make up the European Union. The vaccine developed by Moderna and the National Institute of Allergy and Infectious Diseases (NIAID), which is also an mRNA vaccine, is currently authorized in 36 countries. These include the U.S., the U.K., and E.U. countries. Sputnik V, which is a viral vector vaccine developed by the Russian research institute Gamaleya, is authorized in eight countries: Algeria, Argentina, Belarus, Bolivia, Guinea, Russia, Serbia, and West Bank. Close on its heels is the Oxford-AstraZeneca viral vector vaccine, which has gained use authorization in seven countries. These are Argentina, the Dominican Republic, El Salvador, India, Mexico, Morocco, and the U.K. Other vaccines that have gained authorization in certain countries are:
At a global forum held on January 15, 2021, Dr. Tedros Adhanom Ghebreyesus — the World Health Organization's (WHO) director-general — said:
The U.K. has been enforcing new lockdowns in the face of ever-increasing cases of COVID-19. These rising numbers may be due to a new, and seemingly more infectious, variant of SARS-CoV-2. South Africa and Brazil have also reported the emergence of new variants that have led to some concern. One of the main questions that people around the world are asking in relation to emerging variants of SARS-CoV-2 is this: Will COVID-19 vaccines be effective against them? So far, specialists and the pharmaceutical companies that produce currently available vaccines have expressed optimism that the vaccines will be effective against emerging variants and strains. When speaking to Medical News Today earlier this month, both Pfizer and the NIAID declared that there is no reason to suspect that their vaccines would not work against the SARS-CoV-2 variant identified in the U.K. "At present, NIAID scientists believe that the SARS-CoV-2 vaccines supported by Operation Warp Speed will provide protection against SARS-CoV-2 [U.K. variant], including […] Moderna and Pfizer-BioNTech COVID-19 vaccines authorized for emergency use by the U.S. Food and Drug Administration [FDA]." Both Pfizer-BioNTech and Moderna-NIAID, whose vaccines are currently authorized for use in the U.S. and U.K., offer mRNA vaccines. These contain genetic information from the virus. Our cells then make the viral Spike protein encoded in this information and present it to our immune system. This, in turn, allows our immune system to "learn" to fight off the virus, which will equip us for future infections with SARS-CoV-2. According to experts, mRNA technology is adaptable enough that, in theory, scientists could easily "tweak" mRNA vaccines so as to ensure effectiveness against emerging variants or strains of a virus. Dr. Uğur Şahin, the CEO of BioNTech, has declared that the Pfizer-BioNTech vaccine should work against different variants of SARS-CoV-2, against which his colleagues have already tested the vaccine. He has also noted that, in any case, their vaccine is easily adaptable. Other scientists have also noted that at least some of the COVID-19 vaccines that have gained authorization around the world should be adaptable so as to remain effective against emerging variants of SARS-CoV-2. In relation to the variant that emerged in South Africa, Dr. Julian W. Tang — a clinical virologist from the University of Leicester in the U.K. — has commented:
"Meanwhile," he added, "most of us believe that the existing vaccines are likely to work to some extent to reduce infection/transmission rates and severe disease against both the U.K. and South African variants — as the various mutations have not altered the S protein [which helps the virus gain entry into healthy cells] shape that the current vaccine-induced antibodies will not bind at all." Although some vaccines have already gained use authorization in various countries, there are still many vaccine candidates currently undergoing clinical trials. Some of the candidates in late-stage trials are showing promise, offering hope that more vaccines may become available around the world by the end of 2021. A top contender is the vaccine candidate developed by pharmaceutical company Johnson & Johnson. This candidate is also known as the Janssen COVID-19 vaccine candidate. Johnson & Johnson's experimental viral vector vaccine uses a modified adenovirus, or a common cold virus, as the vaccine candidate "base." This carries the gene for the SARS-CoV-2 Spike protein. Unlike some of the vaccines that have already gained use authorization, the company are testing this vaccine candidate as both a single-dose and a two-dose regimen to create immunity. The Janssen COVID-19 vaccine candidate was already showing some promise in early trials, though these briefly paused in October 2020 due to one of the trial participants developing "unexplained illness." Trials have since resumed, and the company have recently made available the interim results from phases 1 and 2. These results indicate that the vaccine candidate was well tolerated by participants overall, suggesting that it is safe. The vaccine candidate also appeared to induced an immune response in those who received it, suggesting that it may also be effective against SARS-CoV-2. The phase 3 trial data should also be available by the end of January, according to a Johnson & Johnson statement. Once these data are available, the company are hoping to file for FDA emergency use authorization. According to a recent New York Times report, Dr. Paul Stoffels — the chief scientific officer at Johnson & Johnson — has commented that "hopefully somewhere in March [the company will] be able to contribute" to vaccination efforts in the U.S. For live updates on the latest developments regarding the novel coronavirus and COVID-19, click here. |
| Is it ethical to continue COVID-19 vaccine trials? - Medical News Today Posted: 04 Jan 2021 12:00 AM PST  The recent authorization of two highly effective COVID-19 vaccines for emergency use in the United States poses an ethical dilemma for researchers conducting ongoing clinical trials. In particular, what is their responsibility toward participants who received placebo injections? All data and statistics are based on publicly available data at the time of publication. Some information may be out of date. Over the past few weeks, the Food and Drug Administration (FDA) have given emergency use authorization (EUA) to two COVID-19 vaccines, one by Pfizer-BioNtech and one by Moderna. As a result, in the coming months, millions of the most vulnerable people in the U.S. will receive a vaccine that protects them against the disease. This is good news, but it does pose an ethical dilemma for researchers conducting ongoing clinical trials of these and other COVID-19 vaccines. More than 180 candidate vaccines against the disease are in development, with at least 12 in phase 3 clinical trials. Clinical trials investigate whether or not a vaccine is safe and effective by giving it to around half of all the volunteers (and giving a placebo vaccination to the rest). The trials are "double blind," meaning that neither the participants nor the researchers know which participants received the vaccine and which received the placebo. According to guidance issued by the FDA in June 2020, in the event of a COVID-19 vaccine being judged safe and effective, there may be a case for "unblinding" trials and offering the vaccine to those who received the placebo. Given that the treatment options remain limited for anyone who develops a severe, life threatening case of COVID-19, it may be in the best interests of trial participants to receive one of the two proven vaccines as soon as possible. Is it, therefore, unethical to continue placebo-controlled clinical trials of these two vaccines? Also, should researchers use placebos in trials of other COVID-19 vaccines? Bioethicists at the National Institutes of Health (NIH) Clinical Center in Bethesda, MD, address these complex ethical issues in an opinion piece in the latest issue of the journal Science.
The authors emphasize that vaccine researchers need to take other factors into consideration when they decide whether or not to continue trials as originally planned. They write that even if early results have found some vaccines to be safe and effective, continuing to conduct trials may bring further benefits for society. For example, due to the challenges of manufacturing sufficient quantities as rapidly as possible, several different vaccines may be necessary to meet global demand. Also, in parts of the world with poor health infrastructures, vaccines that need to be stored and transported at very low temperatures — as is the case for the Pfizer-BioNTech vaccine — are impractical. In addition, some vaccines may be more effective than others at protecting particular groups, such as older people or those with comorbidities. "This highlights the potential social value of conducting additional trials after one or more vaccine candidates are found to be safe and efficacious," they write. Even after the FDA grant EUA to a vaccine, conducting further research may provide additional information and reassurance about its safety and efficacy before offering it to millions of people. Some commentators argue that once a clinical trial has gathered enough data to show that one arm of the trial is superior to the other — or superior to what is available outside the trial — it is no longer ethical to continue the research. According to this view, the authors write, "researchers conducting clinical trials are obligated to treat participants consistent with their clinical interests," and so it is no longer ethical to give participants a placebo once scientists have identified a safe and efficacious vaccine. "We disagree," they write. "This view fails to recognize that the obligations researchers have to their participants are distinct from the obligations that clinicians have to their patients." They point out that there are mechanisms in place to protect people who take part in clinical trials. For example, volunteers must give their informed consent before they can participate. In addition, an independent board known as an Institutional Review Board will only approve plans for trials if they consider the balance of individual risks and potential social benefits to be acceptable. The authors say that it can be ethically appropriate to invite participants to accept some risks in order to collect data that benefit wider society. They write:
They list several social benefits that continuing trials may provide, including:
They conclude:
Even if experts judge the risks to participants to outweigh any potential benefits, particularly for medically vulnerable individuals, they write that researchers still have several options. Among these are "unblinding" the trial and offering the vaccine to participants who received the placebo, then following them up to collect additional data. Finally, they note that researchers who are designing new clinical trials might consider comparing their vaccine candidate with one of the authorized COVID-19 vaccines rather than a placebo. For live updates on the latest developments regarding the novel coronavirus and COVID-19, click here. |
| You are subscribed to email updates from "poliomyelitis treatment" - Google News. To stop receiving these emails, you may unsubscribe now. | Email delivery powered by Google |
| Google, 1600 Amphitheatre Parkway, Mountain View, CA 94043, United States | |

Comments
Post a Comment